Recent breakthroughs in TIM-3 Alzheimer’s research have unveiled exciting prospects for combating this debilitating disease. The research highlights how a checkpoint molecule known as TIM-3 potentially plays a crucial role in Alzheimer’s treatment by regulating microglial function in the brain. By inhibiting the expression of TIM-3, scientists have found that these immune cells can efficiently clear amyloid plaques, which are notorious for impairing cognitive function. This innovative approach borrows from successful immune system strategies used in cancer therapies, providing hope for enhanced Alzheimer’s treatment options. As the scientific community delves deeper into the TIM-3 mechanism, the potential to reverse cognitive decline and restore memory could become a reality for millions suffering from this condition.
Exploring the intersection of immunology and neurodegeneration, TIM-3 Alzheimer’s research opens new pathways in the quest for effective treatments. The TIM-3 molecule, an inhibitory checkpoint, facilitates a unique relationship between the immune system and brain health, particularly in the context of Alzheimer’s disease. Research has revealed that modulating this checkpoint can enhance the immune response in the brain, allowing immune cells like microglia to better address the accumulation of toxic plaques. By understanding how TIM-3 affects immune activity, researchers could potentially design therapies that mimic anti-TIM-3 strategies, translating insights from cancer immunity to neurodegenerative outcomes. This intersection of knowledge could redefine approaches to mitigate the impacts of Alzheimer’s and improve overall brain health.
Understanding the TIM-3 Mechanism in Alzheimer’s Disease
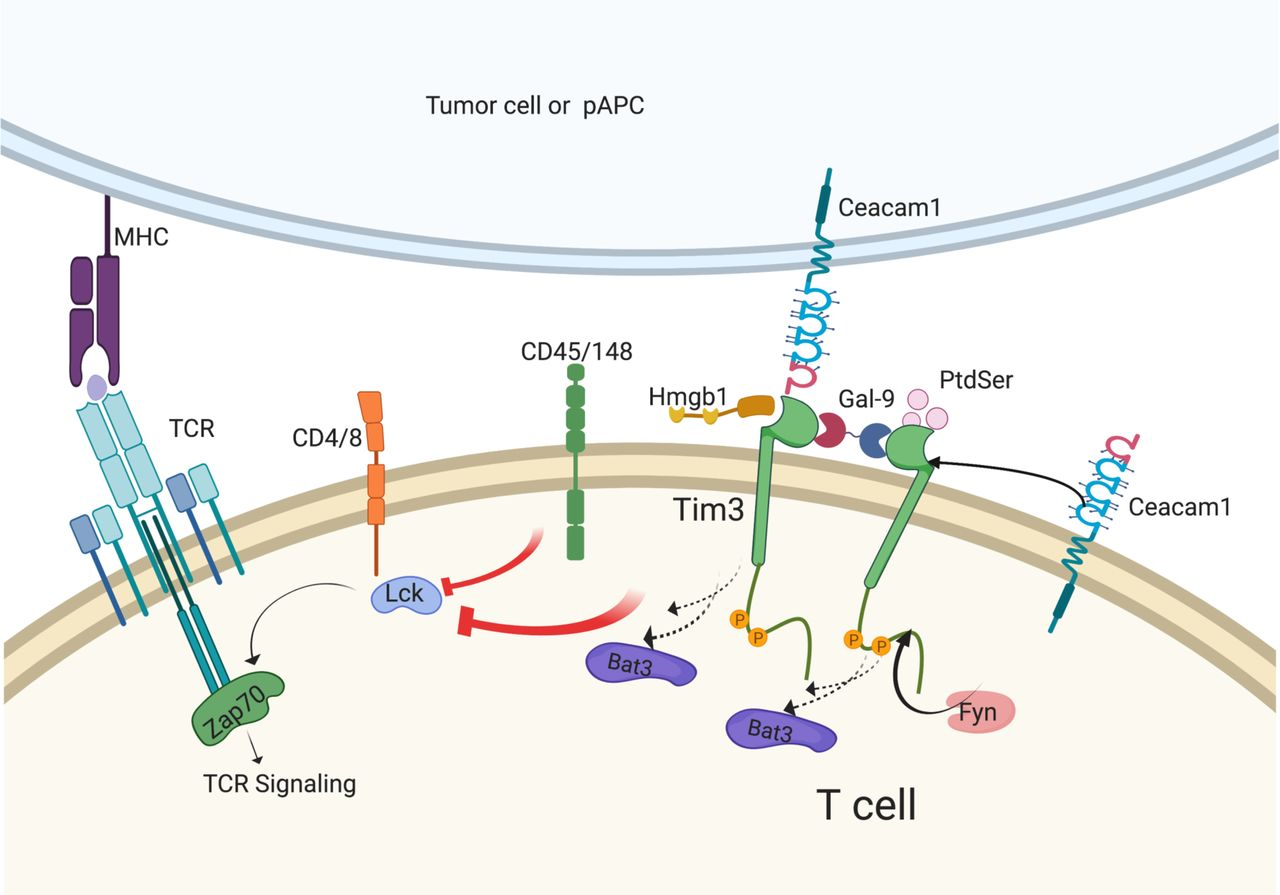
The TIM-3 molecule plays a critical role in the pathophysiology of Alzheimer’s disease (AD). Recent studies have indicated that TIM-3 expression is significantly elevated on microglia in AD patients, which directly correlates with decreased clearance of amyloid-beta plaques from the brain. This suppression of microglial activity thanks to TIM-3 leads to plaque accumulation, contributing to cognitive decline. By understanding the mechanism behind TIM-3’s inhibitory effects, researchers can begin to formulate therapeutic strategies that leverage this knowledge to promote microglial activity and enhance plaque clearance.
In essence, TIM-3 functions as a regulatory checkpoint within the immune system, which can inadvertently contribute to the progression of Alzheimer’s disease. By blocking TIM-3, it is possible to free microglia from their inhibited state, fostering an environment where these immune cells can effectively engage and clear the harmful plaques that characterize AD. This approach highlights the potential of TIM-3 as a promising target in developing innovative treatments aimed at combatting Alzheimer’s symptoms.
Reimagining Alzheimer’s Treatment: Anti-TIM-3 Therapy
The development of anti-TIM-3 therapy presents an exciting avenue for treating Alzheimer’s disease. By utilizing antibodies designed to block TIM-3, researchers aim to enhance microglial function, thereby enabling these immune cells to actively participate in the phagocytosis of amyloid-beta plaques. This shift from symptom alleviation to tackling the root cause of plaque accumulation may improve outcomes for patients suffering from Alzheimer’s disease. Existing anti-TIM-3 antibodies, originally designed for cancer treatments, could be repurposed, highlighting a potential shortcut in the drug development process.
Initial animal studies suggest that when TIM-3 is inhibited, microglia not only increase their activity towards plaque clearance but also improve cognitive functions in models of late-onset Alzheimer’s disease. These breakthroughs evoke optimism in a field that has faced significant challenges with previous therapeutic interventions. Given the demonstrated link between TIM-3 modulation and improved cognitive outcomes in mice, further research into anti-TIM-3 therapies could pave the way for new, effective treatments that alter the trajectory of Alzheimer’s disease.
The Role of Microglia in Alzheimer’s Disease Pathogenesis
Microglia are integral to the brain’s immune response and are pivotal in maintaining neuronal health. When functioning optimally, they clear debris, regulate synaptic connections, and respond to harmful stimuli. However, in Alzheimer’s disease, microglial activation often results in an exacerbation of neuroinflammation, where impaired clearance of amyloid plaques leads to further damage and neurodegeneration. Understanding the duality of microglial function is essential to developing strategies that can modulate their activity without compromising their protective roles.
As research continues to unravel the complexities of microglial function, the importance of managing their activation states becomes clear. Approaches that can restore their ability to clear amyloid plaques in the context of Alzheimer’s, while avoiding detrimental inflammatory responses, are crucial. This insight into microglial roles not only enhances our understanding of AD but also underscores the necessity for targeted therapies that harness the beneficial aspects of microglial activity.
Implications of TIM-3 Gene Polymorphisms in Alzheimer’s Risk
Genetic studies have illuminated the role of TIM-3 gene polymorphisms in influencing individual susceptibility to Alzheimer’s disease. These genetic variations can affect the expression of TIM-3, thereby impacting microglial function and the body’s innate ability to clear amyloid plaques. For instance, individuals carrying specific polymorphisms may present with higher levels of TIM-3 on microglia, which could lead to reduced plaque clearance and an increased risk of developing Alzheimer’s disease.
Understanding how TIM-3 gene polymorphisms relate to Alzheimer’s risk not only aids in identifying high-risk individuals but also opens potential pathways for personalized medicine. By considering a patient’s genetic profile, therapeutic strategies can be tailored to enhance microglial activity and improve clinical outcomes. This approach signifies a move toward precision medicine in Alzheimer’s research, where genetic factors are pivotal in guiding treatment options.
Future Directions: TIM-3 Research and Alzheimer’s Disease
The future of Alzheimer’s disease research is increasingly focused on targeting immunological pathways, particularly through molecules like TIM-3. With promising data emerging from animal models, the next steps involve validating these findings in human studies. Researchers are eager to ascertain whether therapeutic blocking of TIM-3 can indeed replicate the cognitive improvements observed in mice, paving the way for clinical trials that could revolutionize Alzheimer’s treatment.
As this area of research evolves, collaboration between neurologists, immunologists, and geneticists will be essential in advancing our understanding of TIM-3 and its wider implications on Alzheimer’s disease. The goal is to build a comprehensive picture of how immune checkpoints like TIM-3 can be manipulated to foster plaque clearance, optimize microglial function, and ultimately improve patient outcomes.
The Importance of Immune System Modulation in Alzheimer’s Treatment
Modulating the immune system has emerged as a cornerstone in the search for effective Alzheimer’s treatments. The intricate dance between protective and harmful immune responses is crucial; while immune activation is necessary for clearing plaques, excessive or inappropriate activation can exacerbate neurodegeneration. By targeting immune checkpoints like TIM-3, which mediates this balance, researchers are paving the way for new therapies that may not only slow disease progression but also restore cognitive function.
The modulation of immune responses also raises questions about personalized treatment approaches that consider an individual’s immune profile. Understanding how the interplay between immune checkpoints and Alzheimer’s pathogenesis varies among patients can lead to targeted interventions that optimize therapeutic outcomes. This focus on immune system modulation signifies a progressive shift towards integrated treatment approaches that encompass neurobiology, immunology, and patient-specific factors.
Challenges in Translating TIM-3 Research to Clinical Practice
While the promise of TIM-3 research in Alzheimer’s treatment is significant, numerous challenges remain in translating these findings into clinical practice. The transition from laboratory findings in animal models to effective therapies in humans often presents hurdles, including differences in gene expression, immune responses, and the brain’s complex environment. Developing safe, effective anti-TIM-3 therapies requires rigorous testing to ensure that enhancing microglial activity does not inadvertently trigger harmful inflammatory processes.
Moreover, the historical context of drug development in Alzheimer’s disease, marked by high attrition rates in clinical trials, requires an adaptive approach to research and development. Collaborations involving interdisciplinary teams will be crucial to overcoming these barriers, ensuring that insights gained from TIM-3 studies can be effectively harnessed to produce clinically viable therapies for much-needed Alzheimer’s treatments.
Potential Side Effects of Targeting TIM-3 in Alzheimer’s Therapy
As with any therapeutic intervention, targeting TIM-3 carries potential risks and side effects that necessitate careful consideration. While inhibiting TIM-3 may enhance microglial activity and plaque clearance, it might also lead to unintended consequences such as overstimulation of the immune response, which could result in neuroinflammation or autoimmunity. Understanding these risks is essential in developing targeted TIM-3 therapies that optimize patient safety and efficacy.
Continuous monitoring and assessment of side effects will be vital during the clinical testing of anti-TIM-3 therapies. Future research must prioritize safety profiles alongside efficacy outcomes to develop robust treatment protocols that minimize adverse events while maximizing cognitive and functional benefits for Alzheimer’s patients.
Comparative Insights: Cancer Treatments and Alzheimer’s Therapies
The intersection between cancer immunotherapy and Alzheimer’s treatment, particularly through TIM-3 modulation, presents intriguing insights and opportunities. Cancer therapies have successfully utilized checkpoint inhibitors to activate immune responses against tumors; similarly, using TIM-3 inhibitors to invigorate microglial function in Alzheimer’s offers a compelling parallel. Both fields emphasize the significance of the immune system’s regulation, suggesting that successful strategies in oncology could inspire new avenues in neurodegenerative disease treatment.
However, the transition from cancer therapies to Alzheimer’s treatments is not straightforward and requires thorough investigation into how these immune mechanisms function in different diseases. Collaboration between oncologists and neuroscientists can yield comprehensive insights into effective strategies that are mindful of the unique pathophysiology of Alzheimer’s disease, ultimately fostering innovations that transcend traditional treatment boundaries.
Frequently Asked Questions
What is the TIM-3 mechanism in Alzheimer’s research?
The TIM-3 mechanism involves the inhibition of microglia, the brain’s immune cells, which prevents them from clearing amyloid plaques in Alzheimer’s disease. By deleting the TIM-3 gene in mouse models, researchers found that microglia can effectively attack and remove these plaques, improving cognitive function in tests.
How might TIM-3 influence future Alzheimer’s treatment strategies?
TIM-3 may provide a novel approach to Alzheimer’s treatment by using anti-TIM-3 therapies that block its inhibitory function. This could enhance the ability of microglia to clear amyloid plaques, potentially improving memory and cognitive function in Alzheimer’s patients.
What role do microglia play in Alzheimer’s disease concerning TIM-3?
Microglia are critical immune cells in the brain that normally help prune away unnecessary synapses. In Alzheimer’s, increased expression of TIM-3 on microglia hinders their ability to clear amyloid plaques, contributing to disease progression and cognitive decline.
How does TIM-3 function as a checkpoint molecule in the immune system?
TIM-3 acts as a checkpoint molecule that regulates immune response by inhibiting overly aggressive immune activity. While beneficial for preventing autoimmunity, its elevation in microglia during Alzheimer’s prevents effective clearance of harmful plaques.
What are the implications of TIM-3 research for Alzheimer’s and cancer treatments?
TIM-3 research suggests potential cross-application of cancer immunotherapy strategies to Alzheimer’s disease. Since TIM-3 plays a role in the immune response, therapies targeting TIM-3 may open new avenues in treating both Alzheimer’s and certain cancers.
Why is TIM-3 considered a genetic risk factor for Alzheimer’s disease?
TIM-3 is linked to late-onset Alzheimer’s through a particular polymorphism in the HAVCR2 gene. This genetic alteration can lead to increased expression of TIM-3, affecting microglial function and plaque clearance in the brain.
What were the primary findings of the TIM-3 Alzheimer’s research conducted at Harvard?
The primary findings highlighted that deleting the TIM-3 gene in mice enhanced the ability of microglia to attack amyloid plaques, leading to improved memory function, thus showing the potential of TIM-3 inhibition as a strategy for treating Alzheimer’s.
How could anti-TIM-3 therapy specifically benefit Alzheimer’s patients?
Anti-TIM-3 therapy could benefit Alzheimer’s patients by restoring the microglial function, enabling them to clear amyloid plaques more efficiently and potentially slowing cognitive decline associated with the disease.
What experimental methods were used to study TIM-3’s effects on Alzheimer’s?
Researchers used genetically modified mice with the TIM-3 gene deleted to study its effects on microglial activity and plaque clearance. Behavioral tests assessed cognitive function improvement as a result of the altered TIM-3 expression.
What is the potential timeline for TIM-3 therapies to reach human trials for Alzheimer’s?
While the timeline is uncertain, researchers are currently testing human anti-TIM-3 antibodies in Alzheimer’s mouse models. If successful, this could pave the way for human clinical trials in the coming years, subject to regulatory approval.
| Key Point | Details |
|---|---|
| TIM-3 Role in Alzheimer’s | TIM-3 is a checkpoint molecule that inhibits immune response, preventing microglia from clearing amyloid plaques associated with Alzheimer’s. |
| Study Findings | Research showed that deleting TIM-3 from microglia allowed them to attack plaques, improving memory in mice. |
| Late-Onset Alzheimer’s | 90-95% of Alzheimer’s cases are late-onset. TIM-3 is linked to genetic risk factors for these cases. |
| Microglia Function | Microglia serve as the brain’s immune cells, but their function diminishes as TIM-3 keeps them from clearing harmful plaques. |
| Future of TIM-3 Therapy | Potential therapies may involve anti-TIM-3 antibodies that could restore microglial function in humans. |
Summary
TIM-3 Alzheimer’s research uncovers a compelling avenue for treating Alzheimer’s disease by utilizing immune checkpoint inhibitors originally developed for cancer therapy. This groundbreaking approach demonstrates that by inhibiting TIM-3, microglia can effectively target and remove harmful plaques in the brain, potentially restoring cognitive function. Given the high prevalence of late-onset Alzheimer’s and the genetic associations with TIM-3, this research may forge a path toward innovative treatments that enhance brain health and memory in affected individuals.