CRISPR gene editing represents a revolutionary leap in biotechnology, offering scientists the unprecedented ability to modify DNA with precision. This cutting-edge technology holds the promise to alleviate genetic disorders like sickle cell disease, transforming lives in ways once thought impossible. However, alongside these advancements arise complex ethical dilemmas that compel us to ponder the ramifications of genetic modification. As we navigate the landscape of CRISPR technology, questions surrounding gene editing ethics, health equity, and the implications of altering human genetics demand critical examination. The delicate balance between innovation and responsibility must guide our approach to harnessing the full potential of CRISPR gene editing in a just and equitable manner.
Gene editing, often referred to as genetic engineering, encompasses a set of techniques aimed at altering the genetic material within organisms. At the forefront of this evolution is CRISPR technology, a powerful tool that facilitates the precise editing of an organism’s genome. This method not only opens doors for groundbreaking treatments of diseases such as sickle cell but also ignites discussions about the ethical considerations of modifying human traits. With the increasing capability to engineer our genes, society is faced with pivotal debates on genetic modification and health equity. These conversations are essential as we ponder the future of our genetic makeup and the responsibilities that accompany such powerful innovations.
Understanding CRISPR Gene Editing: A Revolutionary Tool
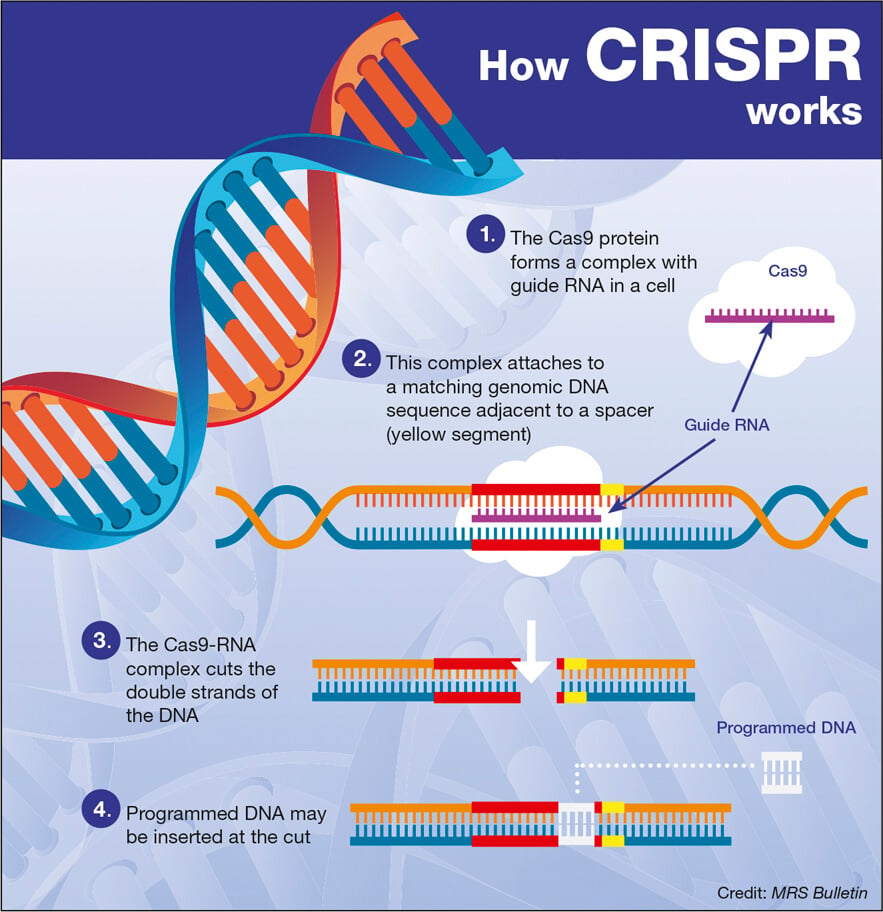
CRISPR gene editing has emerged as a groundbreaking biotechnological tool that allows scientists to modify the genetic material of living organisms easily and precisely. This technology operates on a fundamental principle where specific DNA sequences can be targeted, cut, and replaced, enabling the alteration of genes associated with various diseases. With its ability to edit both somatic and germline cells, CRISPR not only offers the potential for curing hereditary conditions but also raises profound ethical implications regarding the manipulation of human genetics.
The application of CRISPR technology in treating genetic disorders such as sickle cell disease heralds a new era in medicine, presenting the possibility of eradicating genetic diseases entirely. However, the ease of use that accompanies CRISPR raises significant ethical questions, primarily surrounding informed consent and access to such treatments. This is particularly crucial in a healthcare landscape marked by disparities, where the price tag for gene editing represents a considerable obstacle for many families.
Ethical Considerations in Gene Editing
The ethical implications of gene editing, especially using CRISPR technology, cannot be understated. As scientists gain the ability to edit genes, they must consider the moral ramifications of their actions. At the forefront of these discussions is the question of whether it is appropriate to correct genetic traits that are not necessarily harmful. For instance, while curing sickle cell disease is beneficial, the prospect of editing the genes of embryos to eliminate traits like the predisposition to Down syndrome brings a host of ethical dilemmas. Who gets to decide which traits are desirable or undesirable?
Moreover, ethical concerns about gene editing extend to issues of health equity. Innovations in gene therapy could create a divide between those who can afford such treatments and those who cannot, exacerbating existing inequalities in healthcare access. As researchers and policymakers navigate the landscape of genetic modification, they must prioritize equitable access to these cutting-edge technologies, ensuring that the potential benefits of CRISPR gene editing are distributed fairly across all segments of the population.
Sickle Cell Disease and Genetic Modification
Sickle cell disease represents one critical area where CRISPR gene editing shows tremendous promise. With gene editing, researchers can target and correct the mutations causing the disease, transforming the lives of affected individuals. This approach involves editing somatic cells to remove the genetic mutations responsible for the disease’s manifestations—strokes and severe pain—which can significantly improve the quality of life for countless patients.
However, the cost of such innovative treatments raises additional ethical concerns. With gene therapy treatment priced at around $2.2 million, questions arise regarding who will bear the financial burden and whether such a groundbreaking solution is accessible to the populations most in need. This elevates discussions around health equity, compelling stakeholders to consider not just the efficacy of treatments but also their accessibility—and the fairness of genetic modification practices in today’s healthcare system.
The Intersection of Innovation and Ethics in Medicine
As CRISPR technology progresses, the medical community finds itself at the intersection of innovation and ethics. While the potential for revolutionary advancements in treating genetic disorders is apparent, it brings with it a slew of ethical considerations that must be addressed. With the power to edit out undesirable traits or diseases, we must reflect on what this means for human diversity and individual autonomy. Are we endorsing a form of genetic selection that could ultimately reshape humanity?
Discussions are increasingly highlighting the need for ethical frameworks that guide the use of gene editing technologies like CRISPR. As Neal Baer pointed out during his talk at Harvard, we cannot ignore the implications of our decisions in the realm of health and medicine. This includes reflecting on the broader social consequences of genetic modification and ensuring that technological advancement does not deepen existing inequities in healthcare but instead, fosters health justice.
Monitoring and Regulation of Gene Editing Technologies
As CRISPR technology continues to evolve, the need for comprehensive oversight and regulation becomes more pressing. Baer raised concerns about the lack of stringent monitoring in countries that may not adhere to established ethical guidelines, such as China and Russia. The potential for unethical practices, including germline editing for non-therapeutic enhancements, necessitates an international conversation about the responsible use of gene editing.
Furthermore, as advancements are made, the medical community must establish clear regulations that ensure gene modification is conducted ethically and safely. This includes advocating for global collaborations to create robust oversight mechanisms that prevent misuse of CRISPR technology. By fostering a dialogue among scientists, ethicists, and policymakers, we can help to navigate the complex ethical landscape while harnessing the benefits of genetic modification for social good.
Reshaping Life: CRISPR and Human Values
The impact of CRISPR gene editing goes beyond the biological realm; it challenges and reshapes our ethical frameworks as humans. By introducing the capability to eliminate genetic diseases, we must consider the implications of such power over human life and the societal values that guide us. For instance, what does it mean to view certain genetic conditions as inherently undesirable, and how does this perspective influence our shared humanity?
Moreover, the values we attach to traits now evaluated through a genetic lens could lead to societal pressures towards conformity. Baer’s reflections on diverse human experiences highlight the necessity of recognizing human variation as a facet of our world that enriches our lives. In a society captivated by innovation, we must engage in ongoing discussions about the values that underpin our actions in genetic modification, ensuring we remain committed to fostering a diverse and inclusive human experience.
Financial Accessibility: A Barrier to Genetic Innovation
While CRISPR gene editing opens doors to innovative treatments that can save lives, the financial barriers associated with these technologies pose a significant challenge. The staggering costs of therapies, such as the $2.2 million price tag for sickle cell disease treatment, raise critical questions about who can access these potentially life-saving solutions. Economic disparities in the healthcare system threaten to widen the gap between those with access to cutting-edge care and those who cannot afford such luxuries.
This issue of financial accessibility sparks a broader discussion about the responsibilities of biotech companies, healthcare providers, and governments. If society is to benefit from advancements in genetic modification, concerted efforts must be made to ensure that financial constraints do not dictate access to healthcare. Advocating for policies that promote equitable distribution of these treatments is essential for realizing the full potential of CRISPR technology for all individuals, regardless of their economic status.
Informed Consent in the Age of Genetic Editing
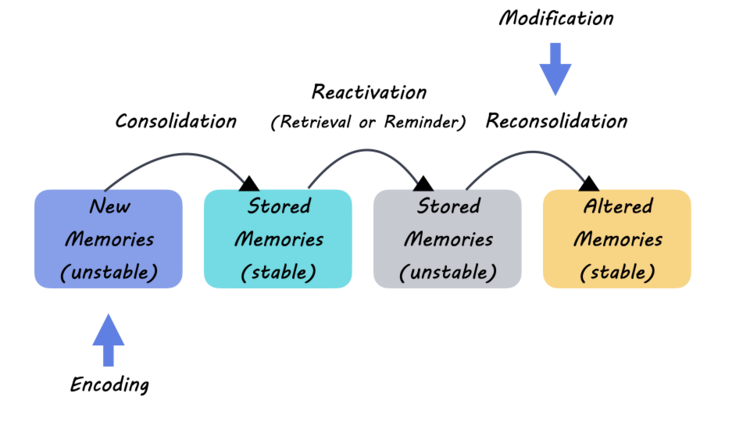
As we dive deeper into the world of CRISPR gene editing, the principle of informed consent emerges as a critical aspect of ethical practice in medicine. Patients and parents must not only be aware of the benefits of genetic modification but also the potential risks and the limits of current scientific understanding. As technology evolves quickly, obtaining truly informed consent poses a challenge, particularly when considering the long-term implications of gene editing.
Establishing clear communication between medical practitioners and patients about the ethical implications and the uncertain outcomes of CRISPR interventions is crucial. This ensures that individuals are empowered to make informed decisions about their health and the health of their offspring. Enhanced focus on ethical education within the healthcare system could ensure that both patients and healthcare providers engage in meaningful dialogues about gene editing’s risks and rewards.
Cultural Perspectives on Genetic Modification
Cultural attitudes towards gene editing vary widely, influencing perceptions of its ethical implications and applications. In certain cultures, the intrinsic value of human diversity may foster acceptance of genetic conditions viewed as part of the human experience. This belief can clash with the biomedical ethos that prioritizes eradicating diseases at any cost. Consequently, understanding cultural perspectives on genetic modification is essential when addressing global health equity.
Incorporating diverse cultural viewpoints can enrich discussions surrounding CRISPR gene editing by broadening the conversation beyond a purely scientific lens. This approach challenges the dominant narratives present in many Western societies, which often focus on technological advancement as an unequivocal good. By engaging with and respecting varying cultural beliefs about health, disease, and what it means to be human, we can create more inclusive discussions and ethical frameworks surrounding the use of gene editing.
Frequently Asked Questions
What are the ethical considerations of CRISPR gene editing?
CRISPR gene editing raises significant ethical questions, especially about who decides what traits are desirable or undesirable. Issues like health equity come into play, as access to gene editing technologies could be limited to those who can afford them, creating disparities in health outcomes. Additionally, the implications of modifying traits in embryos or addressing conditions such as Down syndrome complicate the ethics surrounding genetic modification.
How can CRISPR technology potentially cure sickle cell disease?
CRISPR technology allows for precise editing of genes responsible for sickle cell disease by directly modifying somatic cells. This means that healthcare providers can alter the genes that cause the disorder, potentially eradicating the disease in affected individuals. However, the high cost of treatments and issues surrounding fair access raise important discussions about health equity.
What role does health equity play in the use of CRISPR gene editing?
Health equity is a critical concern in the context of CRISPR gene editing, as the cost of treatments like those for sickle cell disease is exceptionally high. Ensuring that all populations have access to these groundbreaking genetic modifications is essential to prevent widening health disparities. Policymakers and ethicists must consider how to make such technologies universally accessible.
Is it ethical to use CRISPR technology for traits that are not linked to disease?
Using CRISPR for non-disease traits raises profound ethical dilemmas. For instance, should parents have the right to genetically modify their child for preferred characteristics? Such actions could lead to societal pressures and further stratification based on genetic traits, which complicates the ethical landscape surrounding genetic modification.
What are the unintended consequences of CRISPR gene editing?
CRISPR gene editing, while revolutionary, may have unintended consequences due to the complex nature of genetics. Changes to one gene can affect other biological pathways, resulting in unforeseen health issues. The long-term implications of such modifications remain largely unknown, necessitating thorough research and consideration before widespread application.
How does gene editing with CRISPR differ from traditional methods?
CRISPR gene editing differs from traditional genetic modification techniques by offering greater precision and efficiency. CRISPR allows for targeted changes to DNA sequences with minimal off-target effects, making it a powerful tool for researchers. Traditional methods often involve random insertion of genes, which can lead to more unpredictable outcomes.
What safeguards are in place for CRISPR gene editing?
Currently, there are regulations in place that govern the use of CRISPR technology, particularly regarding germline editing. However, enforcement varies globally, and some countries may lack robust oversight. This raises concerns about ethical practices and the potential for misuse of gene editing technologies.
Why is public discourse important in assessing CRISPR gene editing?
Public discourse is vital in assessing CRISPR gene editing because societal values and opinions shape policy decisions around genetic modification. Engaging diverse stakeholders, including ethicists, scientists, and community members, helps ensure that health equity and ethical considerations are prioritized in the development and implementation of gene editing technologies.
| Key Topics | Description |
|---|---|
| CRISPR Technology | A gene-editing tool that allows scientists to alter both somatic and germline genes. |
| Ethical Concerns | Debates surrounding the appropriateness of editing genes that affect human variation and quality of life. |
| Cost Implications | The financial burden of treatments, such as the $2.2 million cost for sickle cell gene therapy. |
| Health Equity | Disparities in access to CRISPR treatments raise questions about fairness in healthcare. |
| Regulation | Concerns about oversight in gene editing practices, especially in countries with lax regulations. |
| Unintended Consequences | Editing genes may lead to unforeseen effects due to genetic interactions. |
Summary
CRISPR gene editing holds the promise of revolutionizing medicine by allowing for the potential cure of genetic diseases like sickle cell anemia. However, this groundbreaking technology also presents significant ethical dilemmas that must be carefully considered. From the cost of treatments and the implications for health equity, to the concerns regarding who gets to decide which genetic traits to alter, the discussion surrounding CRISPR is as complex as it is crucial for the future of healthcare.