Maternal mortality in the US is a growing concern that highlights a significant health crisis. With over 80 percent of pregnancy-related deaths deemed preventable, the rising rates paint a troubling picture, particularly stark among specific racial and ethnic groups. A recent study revealed that the US leads high-income countries in maternal mortality, with alarming disparities seen across states and demographics. Conditions such as cardiovascular disease have emerged as leading causes of these preventable pregnancy deaths, further compounding the urgency for comprehensive maternal health reform. Addressing racial disparities in maternal mortality and improving postpartum care could be pivotal steps toward reducing these tragic statistics.
The issue of maternal mortality in the United States represents a pressing health challenge that demands immediate attention and action. This crisis, marked by a sharp increase in pregnancy-related fatalities, reveals deep-rooted inequalities in health care access and quality, particularly affecting marginalized communities. Researchers have identified both systemic healthcare deficiencies and chronic medical conditions among reproductive-age individuals as contributing factors to this alarming trend. With significant racial disparities and a concerning rise in deaths during the postpartum period, the need for effective policies and support systems cannot be overstated. Arguably, the nation’s approach to maternal health needs a systemic overhaul to prevent predictable and avoidable tragedies.
Understanding Maternal Mortality in the U.S.
Maternal mortality in the U.S. remains a pressing health crisis, dominating the spotlight due to the striking statistic that over 80% of these deaths are preventable. Despite being one of the wealthiest nations, the U.S. consistently reports higher rates of pregnancy-related deaths compared to other high-income countries. This alarming trend is attributed to a fragmented healthcare system, which lacks equitable access to necessary maternal health services. While many other developed nations have successfully reduced mortality through comprehensive prenatal and postpartum care, the U.S. continues to struggle due to persistent systemic issues such as racial disparities and inadequate public health infrastructure.
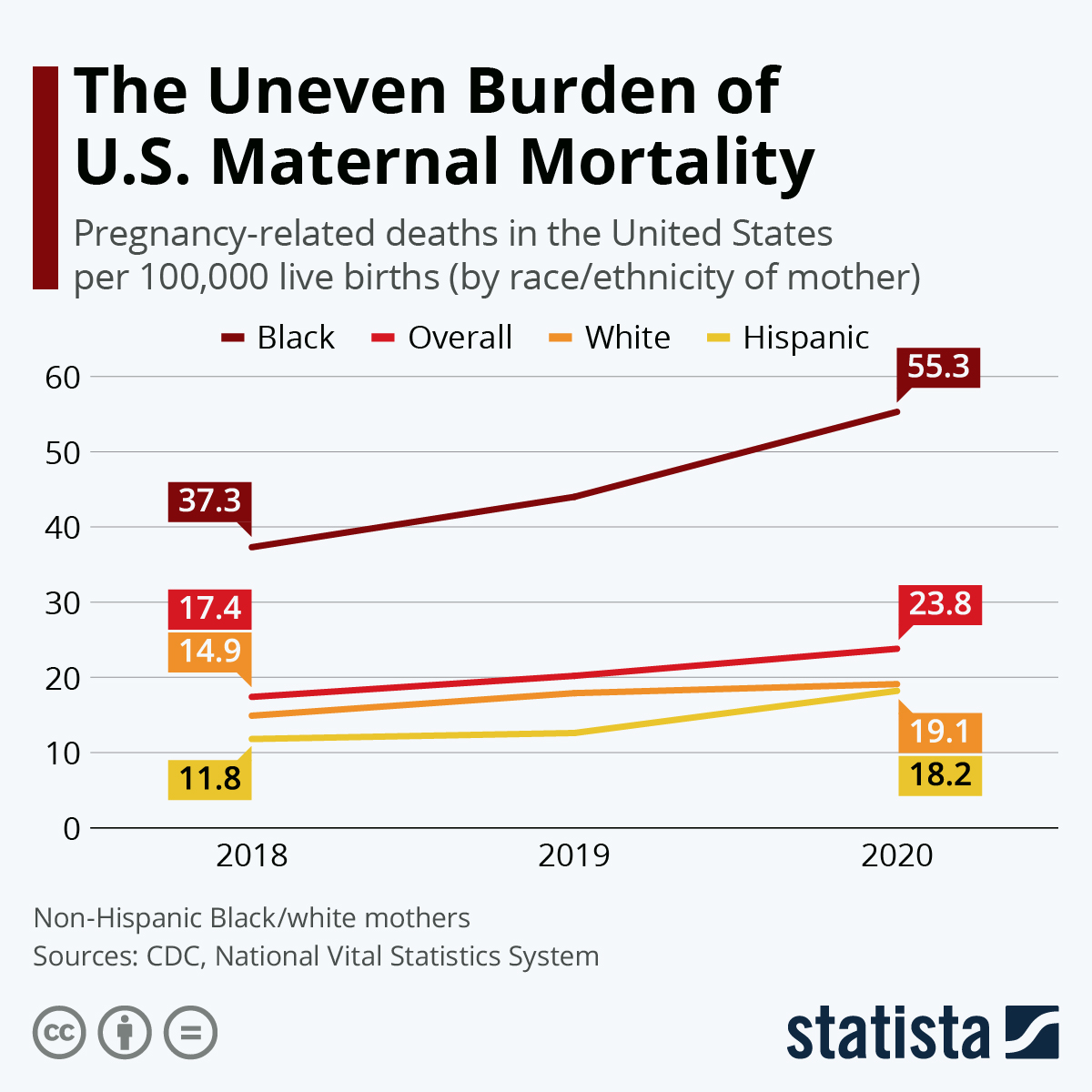
Research reveals that maternal mortality rates vary significantly by race and state, with American Indian and Alaska Native women facing the highest risk. The recent increases in these rates, especially during the COVID-19 pandemic, highlight the urgent need for reform in maternal healthcare. Improved access to care and investment in preventive measures could drastically reduce pregnancy-related deaths, making this issue not only a matter of health but one of social justice as well.
Racial Disparities in Maternal Mortality Rates
Racial disparities in maternal mortality rates present a significant barrier to achieving equitable maternal health outcomes. Data show that non-Hispanic Black women and women of native descent experience markedly higher mortality rates compared to their white counterparts. These disparities arise from a complex interplay of factors, including socioeconomic status, access to quality healthcare, and underlying health conditions that disproportionately affect these populations. For instance, chronic issues like hypertension and diabetes, which can complicate pregnancy, are more prevalent among these groups due to systemic inequities in healthcare access.
Addressing these disparities must focus on creating targeted interventions aimed at improving maternal health outcomes for marginalized communities. Furthermore, healthcare policies should include comprehensive training for healthcare providers to reduce bias and discrimination within maternal health settings. The goal is to ensure that all women, regardless of race or socioeconomic status, receive the quality care they deserve throughout their pregnancy and postpartum periods.
The Importance of Postpartum Care
Postpartum care is a critical aspect of maternal health that is often overlooked despite its importance in preventing maternal mortality. Statistics indicate that nearly a third of all maternal deaths occur in the late postpartum period, from 42 days to one year after childbirth. This gap in care can be particularly harmful if new mothers are not adequately monitored or supported to recover physically and mentally from childbirth. This indicates a need for healthcare systems to extend care beyond the traditional six-week postpartum visit, recognizing the ongoing challenges faced by mothers during the year following delivery.
A comprehensive approach to postpartum care should incorporate mental health support and management of chronic conditions to ensure that mothers are not left to navigate their recovery alone. Increasing investments in postpartum care regimens, along with public health campaigns to educate new parents about the importance of ongoing care, can empower women and reduce the risk of preventable pregnancy deaths. Consequently, efforts must be directed towards making postpartum care more accessible and holistic.
Preventing Pregnancy-Related Deaths Through Quality Care
Preventable pregnancy deaths remain a stark reality in the U.S., underscoring the urgent need for enhanced maternal healthcare practices. Research indicates that the leading cause of pregnancy-related deaths is cardiovascular disease, which can be exacerbated by inadequate prenatal and postpartum care. Effective interventions could significantly reduce this preventable mortality if implemented consistently across all states. This includes improving the quality of care provided before, during, and after childbirth, focusing on risk assessment and patient education.
Additionally, healthcare providers should be trained to recognize warning signs and symptoms that might indicate serious health issues during and after pregnancy. By focusing on early detection and intervention, healthcare systems can help ensure that more women successfully navigate their pregnancy with appropriate medical support, ultimately saving lives. Furthermore, the adoption of best practices shown to work in states with lower maternal mortality rates could be instrumental in addressing systemic inequalities and improving overall maternal health outcomes.
The Impact of Healthcare Access on Maternal Health
Access to quality healthcare is a vital component of maternal health and plays a significant role in influencing pregnancy outcomes. In the U.S., disparities in healthcare access create significant barriers for many women, particularly in rural areas and low-income communities. Maternity care deserts, defined as areas with insufficient obstetric services, contribute to higher rates of maternal mortality, as they prevent women from obtaining timely and necessary care. Addressing these access issues through policy reforms and improved healthcare infrastructure is crucial for alleviating the maternal health crisis.
Efforts to enhance healthcare access must also prioritize underserved racial and ethnic groups, who often face compounded barriers due to systemic racism and economic disadvantage. By actively working to eliminate these barriers, policymakers and healthcare providers can ensure that all women receive the care they need throughout their entire pregnancy journey. This requires a collective commitment to investing in healthcare resources and implementing innovative solutions to reach those who are most at risk of preventable pregnancy deaths.
Lessons from COVID-19 and Maternal Health
The COVID-19 pandemic has highlighted existing vulnerabilities within the U.S. maternal healthcare system and exacerbated challenges in maternal mortality rates. As the pandemic progressed, many pregnant individuals faced increased anxiety due to the uncertainty of healthcare access and resources during this unprecedented time. The significant disruptions caused by COVID-19 have underscored the necessity for a robust healthcare response that is adaptable and capable of meeting the needs of expectant mothers, portraying the importance of continuous care throughout pregnancy and the postpartum period.
Moreover, lessons learned from the pandemic should inform future strategies aimed at improving maternal health outcomes. There is a clear need for integrated care models that encompass mental health support and chronic disease management during pregnancy, especially in times of crisis. By prioritizing maternal health, even in the face of potential disruptions, the healthcare system can work toward reducing preventable pregnancy deaths and ensuring that all mothers have access to safe and effective care.
Innovative Solutions to Maternal Health Crisis
Addressing the maternal health crisis in the United States requires innovative solutions aimed at improving care quality and access. Telehealth services have emerged as a vital resource in bridging gaps in maternal healthcare, providing more women with access to specialists and consultations without the need for in-person visits. This technology can be particularly beneficial for those living in rural areas where healthcare facilities may be limited. By leveraging telehealth, clinicians can monitor patients’ health remotely and intervene early when necessary, which may significantly curb the rates of preventable pregnancy-related deaths.
In addition to telehealth, community-based initiatives that connect women with local health resources can play an essential role in improving maternal health outcomes. Programs that provide education on maternal health and promote awareness of available services can empower women with the knowledge they need to advocate for themselves and seek care when required. Ultimately, pursuing these innovative approaches can help tackle the complexities of maternal mortality, making it possible to cultivate a healthier future for mothers across the country.
The Role of Community Support in Maternal Health
Community support systems play a critical role in enhancing maternal health and reducing mortality rates. The encouragement, emotional and practical support from family, friends, and community organizations can make a significant difference in the experiences of new mothers. Establishing strong networks within communities can create an environment that fosters comprehensive care. When childbirth is surrounded by understanding and resources, women are more likely to seek help for physical and mental health issues that may arise.
Moreover, community engagement can lead to the development of localized programs specifically tailored to meet the needs of diverse populations. Emphasizing community-led solutions enables individuals to express their unique challenges and preferences directly, ensuring that the services provided are relevant and accessible. As a result, integrating community support into maternal healthcare strategies is vital for addressing the broader social determinants of health that contribute to maternal mortality and ensuring that all women have the opportunity for safe and healthy pregnancies.
Advocacy for Maternal Health Reform and Policy Changes
Advocating for comprehensive maternal health reform is essential to combat the rising rates of maternal mortality in the U.S. Policymakers, healthcare providers, and community advocates must collaborate to address the root causes of preventable pregnancy deaths, including inequality in access to care and inadequate postpartum support. A focus on systemic changes can lead to more equitable healthcare outcomes, especially for marginalized groups who are disproportionately affected by high maternal mortality rates. Engaging in policy advocacy can drive change in areas like funding for maternal health programs and improved training for healthcare providers.
Furthermore, elevating the voices of those who have experienced maternal health challenges can inform and shape policies that genuinely address the needs of women. By prioritizing the experiences and recommendations of the communities, stakeholders can implement evidence-based solutions that resonate with the populations they serve. This inclusivity is fundamental in fostering an equitable healthcare landscape aimed not only at reducing maternal mortality but also at nurturing healthier mothers and families across the nation.
Frequently Asked Questions
What are the main causes of pregnancy-related deaths in the US?
In the US, the leading causes of pregnancy-related deaths include cardiovascular disease, hemorrhage, and hypertensive disorders. Cardiovascular complications account for over 20% of these deaths, with rising rates particularly observed among women aged 25 to 39. Issues such as chronic hypertension are becoming more prevalent among younger women, contributing significantly to the maternal mortality crisis.
How does the maternal mortality rate in the US compare to other high-income countries?
The maternal mortality rate in the US is alarmingly high compared to other high-income nations, placing the country at the top of this statistic. Factors contributing to this crisis include a fragmented healthcare system, inequitable policies, and persistent racial disparities in maternal mortality. Despite being a wealthy nation, the US continues to face challenges in providing adequate maternal health care.
What role do racial disparities play in maternal mortality in the US?
Racial disparities significantly influence maternal mortality in the US, with American Indian and Alaska Native women experiencing mortality rates nearly four times higher than white women. Non-Hispanic Black women also face disproportionately high rates of pregnancy-related deaths. These disparities highlight the systemic bias within healthcare systems that needs to be addressed to improve maternal health outcomes.
What is the significance of postpartum care in preventing maternal mortality?
Postpartum care is crucial for preventing maternal mortality as it encompasses the health care received after childbirth. Recent studies indicate that nearly a third of maternal deaths occur between 42 days and one year postpartum, indicating a need for better healthcare systems that extend support beyond the immediate postpartum period to reduce preventable pregnancy deaths.
What are the implications of increasing pregnancy-related deaths in the US?
The rising number of pregnancy-related deaths in the US indicates a maternal health crisis that necessitates urgent action to improve care quality and access during pregnancy and postpartum. Policymakers and healthcare leaders must address disparities, invest in public health infrastructure, and enhance support systems for all mothers to ensure safer pregnancy outcomes.
How do preventable factors contribute to maternal mortality in the US?
Over 80 percent of pregnancy-related deaths in the US are considered preventable. Factors such as inadequate access to healthcare before, during, and after pregnancy, chronic health conditions, and systemic biases contribute to these preventable deaths. Addressing these issues could significantly decrease maternal mortality rates nationwide.
What can be done to reduce maternal mortality in the US?
To reduce maternal mortality in the US, there needs to be a comprehensive approach that includes improving access to prenatal and postpartum care, addressing racial and socioeconomic disparities, increasing public health investments, and implementing evidence-based policies that provide quality maternal care for all women throughout their pregnancy journey.
Why are late maternal deaths an important factor in maternal mortality discussions?
Late maternal deaths, occurring between 42 days and one year postpartum, are crucial to consider because they highlight the need for continuous healthcare support beyond the traditional postpartum period of six weeks. Recognizing and addressing these deaths can lead to improved care strategies and policies that ensure the health of mothers is monitored beyond birth.
| Key Point | Details |
|---|---|
| Current Status | The U.S. has the highest maternal mortality rate among high-income countries, with a rising trend from 2018 to 2022. |
| Preventability | Over 80% of pregnancy-related deaths in the U.S. are preventable. |
| Racial Disparities | American Indian and Alaska Native women face the highest mortality rates at 106.3 per 100,000 live births. |
| Leading Cause of Death | Cardiovascular disease is the leading cause, accounting for 20% of pregnancy-related deaths. |
| Postpartum Deaths | ‘Late maternal deaths’, occurring up to one year postpartum, account for nearly a third of deaths. |
| Importance of Tracking | A consistent national system for tracking maternal deaths was implemented in 2018. |
| Need for Policy Change | Investment in public health infrastructure and increased focus on postpartum care are essential for improvement. |
Summary
Maternal mortality in the U.S. is a pressing public health crisis as new studies reveal a troubling rise in pregnancy-related deaths. Despite having the highest rate among high-income countries and the fact that over 80% of these deaths are preventable, disparities in mortality rates persist across racial and ethnic lines. The need for improved prenatal and postpartum care is urgent, particularly in addressing the chronic health conditions that disproportionately affect young mothers. Effective policy changes and increased funding for maternal health initiatives are crucial to reversing this trend.